Aseptic meningitis is a disease characterized by serous inflammation of the coverings of the brain, often with an accompanying mononuclear pleocytosis. Aseptic meningitis syndrome isn’t caused by pyogenic bacteria. The term aseptic meningitis is not any longer synonymous with viral meningitis, even though the two are still frequently used interchangeably. With a few conditions, the clinical and lab findings accompanying severe viral meningitis are inadequately unique to allow an etiologic analysis, and identifying these problems from the number of nonviral illnesses can be difficult. No specific pharmacological treatment is available for most cases of viral meningitis, these individuals are managed with supportive treatment, which include analgesics, antinausea medicines, intravenous fluids, and prevention and treatment of complications.
Overall, viral infection is the most typical form of aseptic meningitis, and enteroviruses are the most typical viral cause. More than 50 subtypes have now been connected with meningitis. Coxsackieviruses and echoviruses, that are enteroviruses, account for approximately 50% of cases of aseptic meningitis. Certain enteroviruses are more inclined to cause meningitis outbreaks, while some are mainly endemic. Herpesviruses, both herpes labialis and sex organ herpes, may cause meningitis in kids and particularly infants. Mumps was a typical cause of aseptic meningitis in the US until mumps vaccination arrived to use. In several nations, mumps virus remains a typical pathogen in aseptic meningitis.
Aseptic meningitis from HIV occurs mainly during the time of seroconversion. Aseptic meningitis from arboviruses follows geographical and seasonal patterns based on the life cycle of arthropod vectors, animal reservoirs, and their contact with human subjects. Eastern equine encephalitis virus often is observed in Atlantic and Gulf areas, while western equine encephalitis virus is common in the western part of the US. WEEV is accountable for more aseptic meningitis cases than EEEV. Approximately 15% of St Louis encephalitis virus infections result in meningitis. In the rural setting, the infection from SLEV tends to follow the same pattern as WEEV infection.
Approximately 18% of individuals infected with Colorado tick fever develop meningitis. Infection with Venezuelan equine encephalitis virus originally leads to influenza like disease in many people. Only 3% of contaminated individuals are known to develop severe meningitis. LCMV, an arenavirus, is an exceptionally rare reason for meningitis. Transmission of LCMV infection happens by contact with dust or food infected by excreta of rodents. Brucellosis is definitely an infection with a bacterium of one of the Brucella species, often Brucella abortus, Brucella melitensis, Brucella ovis, Brucella suis, or seldom Brucella canis. The occurrence of drug induced meningitis is unknown.
More from Things Health
-
Understanding Rare Forms Of Lung Cancer
One rare type of cancer is called Mesothelioma, a dangerous tumor in the mesothelial tissues of the lungs as well as the abdomen, rising from…
-
Understanding Crohn's Disease
Crohn's Disease is an Inflammatory Bowel Disease commonly referred to as IBD. Inflammatory Bowel Disease consists of several disorders, the primary two are Crohn's Disease…
-
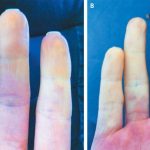
Understanding Raynaud's Disease
Raynaud's disease is a rare disorder of the blood vessels, usually in the fingers and toes. It causes the blood vessels to narrow when you…
-
Symptoms Of A Sinus Infection
Every year, millions of individuals suffer from sinus infections. A sinus infection is merely an irritation or infection of the sinus cavities. The sinus cavities…
-
Living With An Overactive Bladder
Overactive bladder affects millions of individuals all around the world every day. Many individuals take to the web to try and find a natural over…